Popliteal vein compression syndrome the MAIN cause of DVT, unrecognised
- Dr David Grosser
- Jan 7, 2017
- 7 min read

Popliteal vein compression syndrome the MAIN cause of DVT
Dr David M Grosser MB BS FRACS FRCS(London)
Senior Consultant EndoVascular/ Vascular Surgeon,
Gold Coast, Queensland, AUSTRALIA
VERY IMPORTANT NEW WORK.

Affects at least 20% of our Population
Popliteal vein compression syndrome has been described in the medical literature for some 30 years. Only in the last few years has it been looked at seriously as a cause for deep vein thrombosis (DVT), pulmonary embolism (PE) and chronic lower limb venous disease.
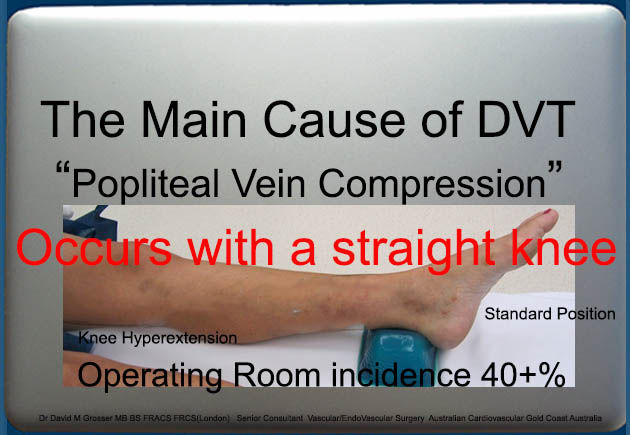
Very simply the popliteal vein lies behind the knee. It is the main deep vein that returns blood from the foot and calf to the heart and lungs for filtering and re-oxygenation. In some people when the knees/legs are extended or straightened fully this vein gets squashed between the layers of muscle behind the knee. This can occur both when standing and sitting or lying with the knee extended. If that position is held for a period of time (for example; in a hospital bed, operating theatre or reading a good book with your legs out on a stool) this can cause blood flow to slow or congest in the calf with little way out. When blood flow slows/stops clotting can occur. This is now beginning to be recognised a major source of deep vein thrombosis for patients undergoing surgery or prolonged bed rest. If the size of the clot is great this can end up filling the heart and lungs. This is called a pulmonary embolus, which can be a life threatening medical emergency.
Popliteal vein compression syndrome however can often be silent, meaning you may not be aware of it until further problems arise. Chronic problems that can occur are most often related to pressure build up in the calves. This can be seen as a dark tan like stain around the lower calf accompanied by thickened dense skin. Development of large varicose veins and venous ulcers can also occur in the later stages. Although it has not been conclusively proven, it is also thought that popliteal vein compression syndrome could also trigger certain types of lung disease through prolonged exposure to multiple small clots arriving in the lungs. We have a collection of patients with pulmonary hypertension with this condition and no other cause to explain the problem.
The popliteal artery can be also become affected but the incidence is very much less. This normally only occurs in those patients with large bulky calf muscles and athletes but some are probably familialy related. The symptoms here can be pain in the calves when walking/running or climbing stairs (atherosclerotic disease causing calf pain is much more common). We have patients referred to us who have total arterial occlusions in both legs below the knees after days in Intensive Care in the supine, leg extended position with later evidence proving vein and artery compression by extension.

From the progressive accumulation of DVT and PE cases that we have discovered associated with this syndrome it appears likely that it is the most significant cause of Thromboembolic Disease,the syndrome and likely explains the major recurrence rate of ThromboEmbolic Disease which at present is labelled "idiopathic ",("the Doctors don't know what is the cause"), (30% of cases being recognised with recurrence within 2 years), and it accounts in large part for severe stasis changes, ulcer disease and the formation of incompetent perforators all of which are not really explained by current theory or data.

I believe that much further work needs to be done but other centres David Huber in Sydney and Luca di Marzo in Rome have been instrumental in explaining the possible significance of this common anatomical trait. It is likely to cause recurrent varicose veins below the knee associated with perforators and is the reason I am sceptical of claims made for really good results from Varicose Vein treatment long term when the Great Vein is only treated above the knee by services who have not recognised or paid any attention to this problem.
It is likely that all the data on prophylaxis of ThromboEmbolism will have to be rewritten and reconsidered. The guidelines are obsolete.
To prevent DVT all hospital beds should have knee flexion incorporated into their structure.
Current guidelines using achilles support to prevent decubitus heel ulcers should be scrapped,
Huber has published demonstrating 40% of patients supine on the operating table with this position have total occlusion of the Popliteal Vein. 20% extra have 80% stenosis a factor of 60% of patients at risk.
Flying. Straight legs encouraged by seating in Economy and now Flat Beds in First Class are probably the major risk of long distance travel.
The current economy class seating does not allow for an average size individual to sit with the knees comfortably flexed, a position is forced with the legs outstretched under the seat in front with the likelihood if the passenger sleeps that there will be a risk of total occlusion of the vein in 20% + with the attendant risks of swelling alone, DVT and or emboli.
We have venograms to show how clot can develop above the knee and not be associated with clot inferiorly, this can allow emboli to occur leaving no evidence in the leg.
The individual may be asymptomatic, or have chest discomfort and shortness of breath or die. Tall Olympic athletes who had Thromboembolic events after their trip to Australia from England may well have had this problem. It is common in Obesity because of Gastrocnemius Muscle Hypertrophy. We have found no evidence at all that it is related to the Popliteal Fossa fat pad as others have proclaimed.
We have patients who have recently upgraded to the first class flat bed facilities who have have been frequent travellers and have had their first Thromboembolic experience associated with this.
All of these problems can occur in your lounge-room, bed, in hospital, long bus or car or train trip if you remain inactive with your knees extended.

Treatment options:
The most common cause of the popliteal vein compression syndrome is due to an additional band of main gastrocnemius muscle (calf muscle).
The band pulls down on the compartment (sheath) that contains the nerve, vein and artery as the leg straightens. Tension can also be increased by flexing or planting the foot at the same time. More than half of the patients we see presenting with acute deep vein thrombosis or other chronic venous disorders demonstrate this problem.
1. First and foremost treatment is to avoid prolonged knee extension whilst sitting and standing.
i. SITTING/LYING:
Maintain a slight knee bend. You can roll your foot and hip out (this naturally bends the knee), or place a pillow underneath the calf. A reclining chair is OK as long the knee joint is bent slightly. If the chair forces the knee straight, place a cushion or pillow lengthways underneath the calf.

ii. STANDING:
If your veins happen to compress in the standing position as well you are likely to have more significant problems; historically blamed on other conditions; and demonstrated as stasis changes in the leg; swelling, oedema, fat necrosis, inflammation, eczema and ulceration with associated perforator incompetence. You will need to try and adopt a stand easy position (if standing still for long periods). This is done by pushing your hips forward slightly and gently bending the knee. You take the weight on the large muscles of the thigh and move your centre of gravity forward slightly. It takes a little while to get used to this. This is particularly important for those that work standing in the one position for hours on end. Compression sox may help control some of the pressure effects in the superficial tissues.
The Knees should be kept flexed slightly, relaxed, at ease at any time there is prolonged inactivity to prevent Popliteal Vein Occlusion.
When standing there is a special muscle developed to allow this, protected from fatiguing the TENSOR FASCIA LATA.
iii. It is a difficult habit to break. If your legs swell and you wish to elevate them to help, please remember to bend the knee. A recent patient has been nursed with his leg up extended after knee surgery. We saw him after 7 months of this management a brightly red swollen painful leg getting worse every day from leg elevation. He was better within days of being told to keep the knee flexed and active.

iv. It may take time for symptoms to improve, especially if this is a chronic problem. However, some patients report dramatic improvement in comfort and leg ache after a few days.
v. Large numbers of patients with chronic ulcers spend their lives with their legs elevated in extension. This is inappropriate unless they have been examined for and had the Compression Syndrome excluded. It is easier to recommend that everyone should keep their knees flexed when still, lying sitting or standing.
2. SURGERY:
In extreme cases where conservative treatment has not worked, such as ongoing leg ulcers or evidence of arterial compression, surgery can be offered. Careful division of the muscle fibers behind the knee can resolve the syndrome. Surgery is not the first option as there are many nerves in the area which have to be very carefully protected to prevent numbness and or weakness of the limb. In our experience as it is so common and can generally be corrected by posture and education once diagnosed , surgical correction should be reserved for repeated DVT, repeated pulmonary emboli, chronic associated lung damage, progressive unexplained pulmonary hypertension, strokes associated with PFO where the PFO cannot be closed, chronic stasis and ulcer problems. persistent swelling and severe recurrent varicose veins associated with recurrent perforators associated with this syndrome.
Current Guidelines for assessment of Vein Problems , Deep and Superficial Veins as used by all Standard Xray Clinics and most Vascular Services prevent this entity from being discovered.
PLEASE CONTACT OUR CLINIC IF YOU HAVE MAJOR VENOUS PROBLEMS PARTICULARLY DVT OR SECONDARY STASIS PROBLEMS, CHRONIC ULCER DISEASE AND MAJOR RECURRENT VARICOSE VEINS WHERE THE CAUSE HAS NOT BEEN PROPERLY EXPLAINED.
THESE ISSUES WILL BE ADDRESSED WITH YOU BY DR GROSSER OR HIS SONOGRAPHER AT THE TIME OF YOUR APPOINTMENT.
WE RECOMMEND REMINDING ANY FRIENDS OR RELATIVES THAT SOMETHING AS SIMPLE AS AVOIDING STRAIGHTENING THE LEGS WHILST GOING ON A LONG HAUL FLIGHT OR DURING PROLONGED BED REST CAN REDUCE THE RISK OF DEVELOPING A DEEP VEIN THROMBOSIS (DVT).
Further information as an explanatory video is available on YouTube :
DR DAVID M GROSSER SENIOR CONSULTANT, VASCULAR AND ENDOVASCULAR SURGERY, AUSTRALIA


























Comments