Level 1, 10 Marine Parade, Southport, QLD, 4215, Australia
Tel: (07) 5531-0355

CAROTID ATHEROMA and STROKE

Carotid Arterial Disease
Carotid Arterial Disease
Atheroma in the Carotid most commonly develops in the BULB Area. Like other areas in the body it tends to be progressive but it is very difficult in any individual to predict the rate of change. As it progressively narrows the risk of stroke increases but many vessels contain complex mixed heterogenous plaque with ulcers which can produce emboli easily. Frequent small emboli can cause diffuse damage initially with few symptoms. Silent Strokes estimated to be five times more common than symptomatic stroke. Larger emboli will cause stroke. We plan treatment when we can predict a significant associated risk.
Clogging of the Carotid Arteries can cause Stroke. When there are symptoms or very severe stenosis the Surgeon can offer treatment with Endarterectomy, Carotid Bypass or Carotid Stenting. Medical Treatment is used for lesser forms of the disease.
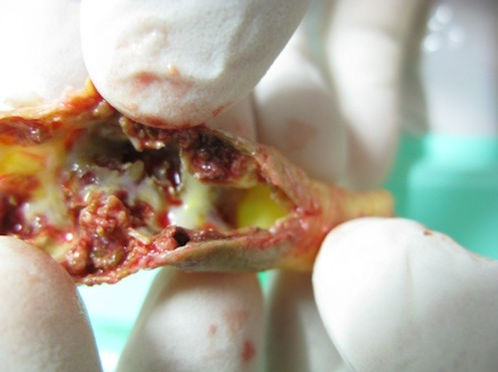
Examples of the atheroma or plaque that can cause stroke.
Page Title

Symptoms
The surgical management of carotid atheroma is often withheld until symptoms occur. These symptoms are usually of the form of a minor or transient stroke and called a T.I.A.
Diagnosis
Diagnosis can be achieved even when there are no symptoms with the use of a simple screening test. This, painless non invasive test is a complex form of Ultrasound allowing visualisation of the vessel, vessel wall and plaque thickness, this is facilitated by the addition of colour flow which is a graphic representation of flow in the vessel. In addition a Doppler flow pattern is combined to measure velocities in the artery. This machine with a good operator can very accurately assess the volume of plaque and the degree of stenosis and so allow a formulation for risk
Prevalence
• PAD is a disease of the arteries that affects 1 million Australians.
• PAD can happen to anyone, regardless of age, but it is most common in men and women over age 50.
• PAD affects 12-20 percent of Australians age 65 and older.
Risk Factors
Testing is appropriate in higher risk individuals and we can provide that in our ultrasound lab.
Your risk of PAD is increased if you are:
• over age 50
• Have a family history of vascular disease, such as PAD, aneurysm, heart attack or stroke
• Have high cholesterol or high lipid blood test
• Have diabetes
• Have ever smoked or smoke now
• Have an inactive lifestyle
• Have a personal history of high blood pressure, heart disease, or other vascular disease
• Have trouble walking that involves cramping or tiredness in the muscle with walking or exercising, which is relieved by resting
• Have pain in the legs or feet that awakens you at night
Treatments
• Lifestyle
Often PAD can be treated with lifestyle changes. Smoking cessation and a structured exercise program are often all that is needed to alleviate symptoms and prevent further progression of the disease.
• Angioplasty and stenting
Initial procedures were performed in the heart in Europe in 1974 and the equipment was progressively redesigned to cope with the more extensive disease and complex situations in the peripheral arteries. The competition between leading companies that supply the engineering and tools to treat this problem has been fierce in the last 15 years and we have lots of amazing equipment that can be applied with small punctures into the arteries rather than extensive open surgery.
This patient presented with rest pain and critical ischaemia in 2001; blocks in Series were treated 2 high grade stenoses stented in 2001 in the SFA artery; angioplasties below the knee:
2007 2 extra stents in SFA but crural vessels remain good and these are still patent in 2013
I have been fortunate to be at the leading edge of these developments since 1980 and participated in the progress from fairly crude balloon devices that were only available in small quantities to todays huge options of large systems to treat aortic stenosis and occlusions in the veins to the very long 200mm plus fine balloons designed to cross through extensive stenoses and occlusions in vessels 2 to 3 mm in diameter below the knee going into the foot.
Using XRay imaging for guidance, we use a fine specially designed wire, to pass through the obstructions, passed into the artery with a puncture and a sheath usually 1.5 to 2mm diameter.
Through the sheath and over the wire that can be considered like a railway line we can pass balloons to open the blockages and stents to support the arterial wall where they are needed. Stent technology continues to progress and there have been dramatic improvements since the 1990s when all that was available were rigid stainless steel stents, large copies of the style being used in the heart.
These rigid stents have been gradually replaced by flexible compressible high radial force stents in keeping with the dynamic forces that have been measured to affect the femoral artery and popliteal especially. The discovery that has allowed this is the development of a special metal alloy of nickel and titanium “Nitinol”. Not all nitinol stents are equivalent and they differ significantly depending on their design characteristics.
The stent is a metal cylindrical device, tiny in the heart arteries and in the arteries below the knee but above the knee to the aorta they can vary between 5 and 32 mm. In some cases especially aneurysms and for stents in the renal arteries a fine polymer covering is used making the device a stent graft.
This management is a minimally invasive treatment that has allowed us to limit the application of open surgery and in most cases I would use this “EndoVascular” approach first.
Blocked Calf Vessels below Complex Popliteal Aneurysm
Double blind trials have shown an equivalent outcome to open surgery but the EndoVascular procedures were carried out with non optimal procedures and the results if carried out with what I have available for routine use now would dramatically change the results in favour of the EndoVascular with a much lower risk of associated morbidity and mortality.
Calf Vessels Recanalised to the foot with Modern angioplasty techniques
Patient returned after this for Pop Aneurysm Repair

Surgery gives better results in the groin region where we often find large masses of occlusive calcium and stents are prone to fracture and failure at this site. Often we can combine Surgical and EndoVascular procedures using Xray in the operating theatre, Special “Hybrid” theatres are being developed to facilitate this and some will have CT scans incorporated to allow assessment during spinal surgery particularly where this involves combined vascular reconstruction.
Particularly in Combined arrangements with Spinal and Vascular Surgeons we have developed procedures that can resolve both the spinal and the vascular components and give a solution that can reduce Multiple Major Surgeries (e.g. aortic aneursym and multiple anterior disk reconstructions) to a Single Operation